When Keratoconus Does the Crime, iDetectives Get There in Time
In a world of ocular diseases, iDetectives are on the case, hunting down sight-threatening conditions and arresting them in their tracks.
#FollowTheClues to help slow or halt the progression of keratoconus…before it’s too late!
Keratoconus care starts with optometry. That’s why it’s critical for optometrists to take on the role of iDetective and look for the clues through a new lens so that patients can be diagnosed as early as possible.
Examination Findings
When your patient history and examination findings present any of the following, consider keratoconus.
Increasing and/or
Unusual Astigmatism
Increase in cylinder ≥1.00 D
Any increase in corneal cylinder or manifest cylinder by 1.00 D or more warrants corneal topography to rule out keratoconus.
Cylinder ≥2.00 D
The suspicion of keratoconus increases significantly in patients with corneal cylinder or manifest cylinder ≥2.00 D.
Irregular, oblique, or ATR astigmatism
Because irregular, oblique, or ATR astigmatism has been associated with keratoconus, topography is therefore highly warranted.
If a patient has ≥2.00 D cylinder in the spectacle prescription, then I question, “Is this a normal cornea?” If the manifest refraction cylinder is ≥2.00 and I see an increase of 1.00 D in cylinder compared to last year, then I highly suspect keratoconus caused this crime.
Increasing and/or
Unusual Astigmatism


From the Case Files of
iDetective Bobby “Eye Spy KC” Saenz
OD, MS, FAAO
iDetective’s Notes:
If a patient has ≥2.00 D cylinder in the spectacle prescription, then I question, “Is this a normal cornea?” If the manifest refraction cylinder is ≥2.00 and I see an increase of 1.00 D in cylinder compared to last year, then I highly suspect keratoconus caused this crime.
From the case files of iDetective
Bobby “Eye Spy KC” Saenz
OD, MS, FAAO
Increasing and/or
Unusual Astigmatism
-
Increase in cylinder ≥1.00 D
Any increase in corneal cylinder or manifest cylinder by 1.00 D or more warrants corneal topography to rule out keratoconus.
-
Cylinder ≥2.00 D
The suspicion of keratoconus increases significantly in patients with corneal cylinder or manifest cylinder ≥2.00 D.
-
Irregular, oblique, or ATR astigmatism
Because irregular, oblique, or ATR astigmatism has been associated with keratoconus, topography is therefore highly warranted.
-
iDetective’s Notes
If a patient has ≥2.00 D cylinder in the spectacle prescription, then I question, “Is this a normal cornea?” If the manifest refraction cylinder is ≥2.00 and I see an increase of 1.00 D in cylinder compared to last year, then I highly suspect keratoconus caused this crime.
-Dr Saenz, iDetective
Unusual Auto-refractor Reading
Error messages
Error messages or unusual findings may result from corneal distortion and irregular astigmatism. Topography may be needed if repeated attempts at measurement fail.
≥0.50 D increase in myopia or MRSE
Keratoconus should be considered if a patient experiences a myopic shift or MRSE change ≥0.50 D from visit to visit. Unexpected changes in prescription could indicate corneal shape changes or steepening, as seen in progressive keratoconus.
Frequent changes in prescription
MRVA worse than 20/20 or repeat complaints about glasses prescription needing to be updated or “being wrong” may indicate keratoconus.
Because most patients are routinely screened using auto-refraction, changes in refractive error may be the first clue of keratoconus. However, presence of refractive error and/or refractive shifts are not mandatory findings of keratoconus.
Unusual Auto-refractor Reading




From the Case Files of
iDetective Tracy “Tracker” Swartz
OD, MS, FAAO
iDetective’s Notes:
Because most patients are routinely screened using auto-refraction, changes in refractive error may be the first clue of keratoconus. However, presence of refractive error and/or refractive shifts are not mandatory findings of keratoconus.
From the case files of iDetective
Tracy “Tracker” Swartz
OD, MS, FAAO

Unusual Auto-refractor Reading
-
Error messages
Error messages or unusual findings may result from corneal distortion and irregular astigmatism. Topography may be needed if repeated attempts at measurement fail.
-
≥0.50 D increase in myopia or MRSE
Keratoconus should be considered if a patient experiences a myopic shift or MRSE change ≥0.50 D from visit to visit. Unexpected changes in prescription could indicate corneal shape changes or steepening, as seen in progressive keratoconus.
-
Frequent changes in prescription
MRVA worse than 20/20 or repeat complaints about glasses prescription needing to be updated or “being wrong” may indicate keratoconus.
-
iDetective’s Notes
Because most patients are routinely screened using auto-refraction, changes in refractive error may be the first clue of keratoconus. However, presence of refractive error and/or refractive shifts are not mandatory findings of keratoconus.
-Dr Schroeder Swartz, iDetective
Unusual
Keratometry (K)
Steepest K >47.00 diopters (D) or radius of curvature <7.2 mm
Average steep K is 43.00-43.50 D. Once steep K is >47.00 D, ectasia should be suspected.
Error messages on auto-keratometry
An error message occurs when the auto-keratometer cannot accurately read an abnormal cornea. Corneal distortion may be the culprit.
Difference of ≥2.00 D between K1 (flat K) and K2 (steep K)
Difference in Ks points to corneal astigmatism. Corneal astigmatism ≥2.00 D correlates to a higher prevalence of keratoconus, which warrants topo-tomography.
Keratometry/auto-keratometry is a keratoconus diagnostic tool available in almost every optometric practice. Watch out for K values >47.00 D, keratometry mire distortion or auto-keratometer error messages, ocular asymmetry between K values, and keratometry values increasing >1.00 D between visits.
Unusual
Keratometry (K)



From the Case Files of
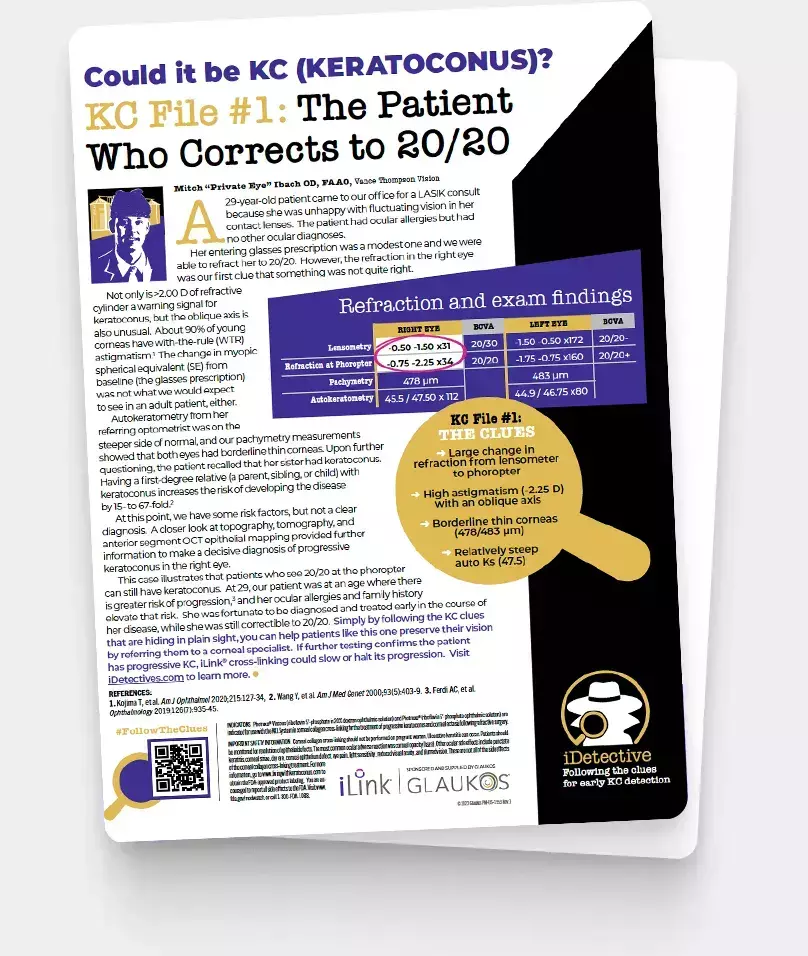
iDetective Mitch “Private Eye” Ibach
OD, FAAO
iDetective’s Notes:
Keratometry/auto-keratometry is a keratoconus diagnostic tool available in almost every optometric practice. Watch out for K values >47.00 D, keratometry mire distortion or auto-keratometer error messages, ocular asymmetry between K values, and keratometry values increasing >1.00 D between visits.
From the case files of iDetective
Mitch “Private Eye” Ibach
OD, FAAO
Unusual
Keratometry (K)
-
Error messages <7.2 mm
Average steep K is 43.00-43.50 D. Once steep K is >47.00 D, ectasia should be suspected.
-
Error messages on auto-keratometry
An error message occurs when the auto-keratometer cannot accurately read an abnormal cornea. Corneal distortion may be the culprit.
-
Difference of ≥2.00 D between K1 (flat K) and K2 (steep K)
Difference in Ks points to corneal astigmatism. Corneal astigmatism ≥2.00 D correlates to a higher prevalence of keratoconus, which warrants topo-tomography.
-
iDetective’s Notes
Keratometry/auto-keratometry is a keratoconus diagnostic tool available in almost every optometric practice. Watch out for K values >47.00 D, keratometry mire distortion or auto-keratometer error messages, ocular asymmetry between K values, and keratometry values increasing >1.00 D between visits.
-Dr Ibach, iDetective

Eye Rubbing &
Ocular Allergy
Eye rubbing is associated with keratoconus
Eye rubbing shows consistent association with keratoconus and keratoconus progression, even though a causal relationship has not been determined. CLEK study findings showed that 50% of keratoconic patients reported eye rubbing in one or both eyes vigorously.1
Atopy is commonly observed with keratoconus
Treating associated atopic eye allergy symptoms may be more effective than asking patients not to rub their eyes.
Other conditions linked with eye rubbing
Vernal keratoconjunctivitis, allergies, atopic dermatitis, dry eye disease, and eye rubbing are all associated with keratoconus.2
References
- Wagner H, Barr J, Zadnik K. Collaborative longitudinal evaluation of keratoconus (CLEK) study: methods and findings to date. Contact Lens Anterior Eye. 2007;30(4):223-232.
- Robati RM, Einollahi B, Einollahi H, Younespour S, Fadaifard S. Skin biophysical characteristics in patients with keratoconus: a controlled study. Scientifica (Cairo). 2016;2016:6789081.
Even in those with no other associated pathology and with negative family history of keratoconus, keratoconus screening with corneal tomography should be considered in children with atopy and eye rubbing behavior, regardless of age.
Eye Rubbing &
Ocular Allergy



From the Case Files of
iDetective Bill “Bond” Tullo
OD, FAAO
iDetective’s Notes:
Even in those with no other associated pathology and with negative family history of keratoconus, keratoconus screening with corneal tomography should be considered in children with atopy and eye rubbing behavior, regardless of age.
From the case files of iDetective
Bill “Bond” Tullo
OD, FAAO
Eye Rubbing &
Ocular Allergy
-
Eye rubbing is associated with keratoconus
Eye rubbing shows consistent association with keratoconus and keratoconus progression, even though a causal relationship has not been determined. CLEK study findings showed that 50% of keratoconic patients reported eye rubbing in one or both eyes vigorously. 1
-
Atopy is commonly observed with keratoconus
Treating associated atopic eye allergy symptoms may be more effective than asking patients not to rub their eyes.
-
Other conditions linked with eye rubbing
Vernal keratoconjunctivitis, allergies, atopic dermatitis, dry eye disease, and eye rubbing are all associated with keratoconus.2
-
iDetective’s Notes
Even in those with no other associated pathology and with negative family history of keratoconus, keratoconus screening with corneal tomography should be considered in children with atopy and eye rubbing behavior, regardless of age.
-Dr Tullo, iDetective
-
References
- Wagner H, Barr J, Zadnik K. Collaborative longitudinal evaluation of keratoconus (CLEK) study: methods and findings to date.Contact Lens Anterior Eye. 2007;30(4):223-232.
- Robati RM, Einollahi B, Einollahi H, Younespour S, Fadaifard S. Skin biophysical characteristics in patients with keratoconus: a controlled study. Scientifica (Cairo). 2016;2016:6789081.
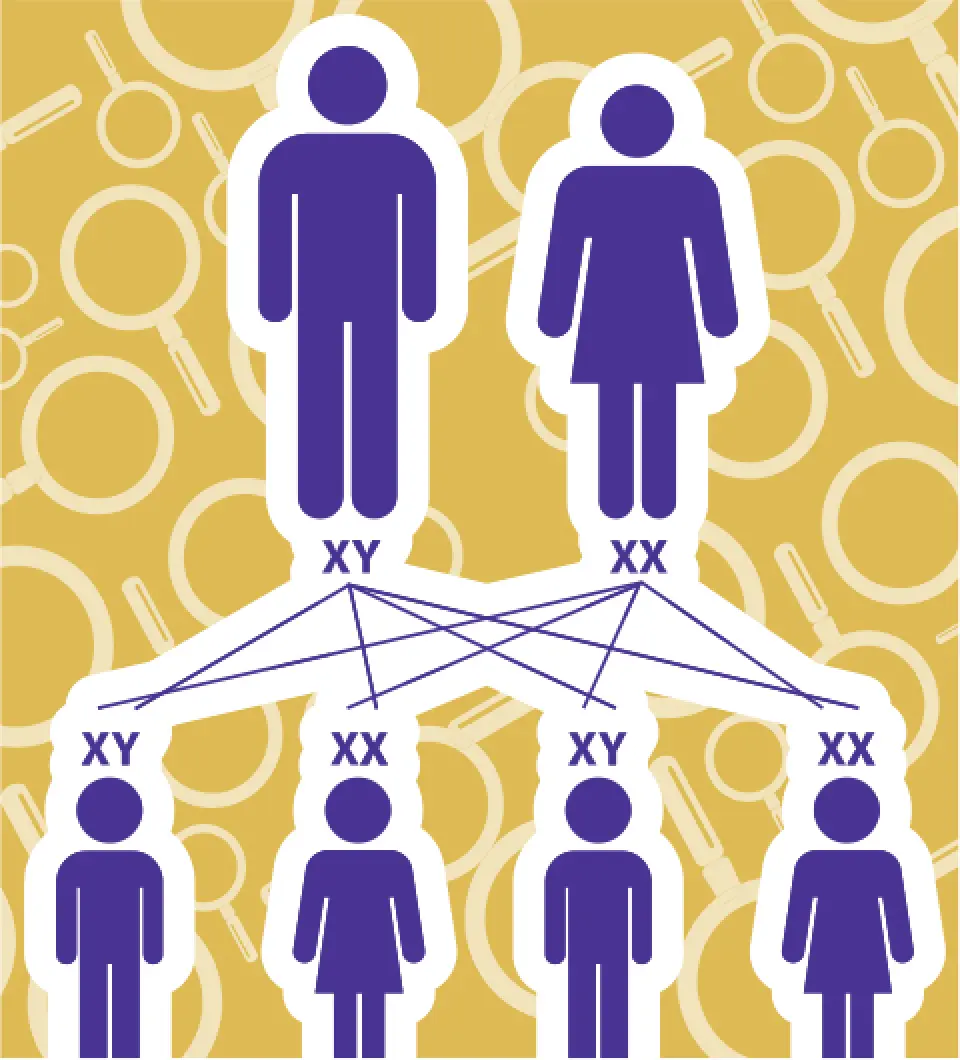
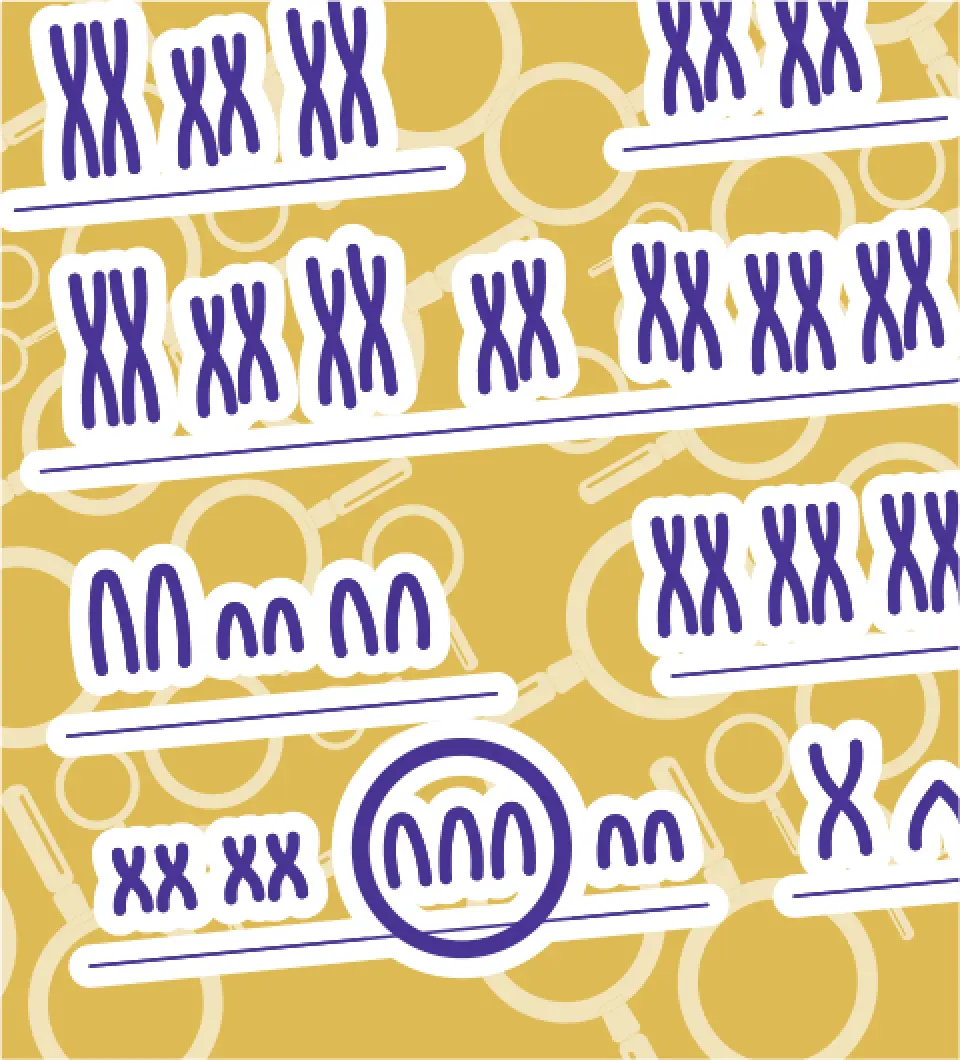
Genetics
Keratoconus is a genetic eye disease
Segregation analysis identifies keratoconus as a complex polygenic disease. There is evidence to associate more than 100 genes with keratoconus.
Keratoconus is found in families
Some studies have reported keratoconus prevalence in first-degree relatives 15 to 67 times greater than in the general population. The CLEK study found that 14% of study patients had a family history positive for keratoconus.1
Reference
- Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015:795738.
Like many diseases, keratoconus results from a combination of genetics and environment. When screening patients, ask if any family members have the condition or other eye problems. A “yes” answer warrants further investigation.
Genetics



From the Case Files of
iDetective Susan “Super Sleuth” Gromacki
OD, MS, FAAO, FSLS
iDetective’s Notes:
Like many diseases, keratoconus results from a combination of genetics and environment. When screening patients, ask if any family members have the condition or other eye problems. A “yes” answer warrants further investigation.
From the case files of iDetective
Susan “Super Sleuth” Gromacki
OD, MS, FAAO, FSLS

Genetics
-
Keratoconus is a genetic eye disease
Segregation analysis identifies keratoconus as a complex polygenic disease. There is evidence to associate more than 100 genes with keratoconus.
-
Keratoconus is found in families
Some studies have reported keratoconus prevalence in first-degree relatives 15 to 67 times greater than in the general population. The CLEK study found that 14% of study patients had a family history positive for keratoconus.1
-
iDetective’s Notes
Like many diseases, keratoconus results from a combination of genetics and environment. When screening patients, ask if any family members have the condition or other eye problems. A “yes” answer warrants further investigation.
-Dr Gromacki, iDetective
-
Reference
- Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015:795738.
Visual Quality
Complaints
Monocular diplopia or ghosting
Keratoconus typically presents asymmetrically. Individuals may notice greater shadowing and doubling of images from the more advanced eye.
Halos and glare
Corneal distortion and higher-order aberrations due to keratoconus may contribute to halos and glare, usually more noticeable at night.
Vision that is not crisp
Irregular astigmatism related to keratoconus makes vision correction difficult with glasses. Further investigate poor quality of vision to rule out ocular disease.
Even with 20/20 vision, the presence of glare or shadows may indicate ocular pathology from the front or back of the eye. Suspect keratoconus in young individuals with worsening visual complaints in the absence of cataracts and retinal disease.
Visual Quality
Complaints




From the Case Files of
iDetective Gloria “Gadget” Chiu
OD, FAAO, FSLS
iDetective’s Notes:
Even with 20/20 vision, the presence of glare or shadows may indicate ocular pathology from the front or back of the eye. Suspect keratoconus in young individuals with worsening visual complaints in the absence of cataracts and retinal disease.
From the case files of iDetective
Gloria “Gadget” Chiu
OD, FAAO, FSLS

Visual Quality
Complaints
-
Monocular diplopia or ghosting
Keratoconus typically presents asymmetrically. Individuals may notice greater shadowing and doubling of images from the more advanced eye.
-
Halos and glare
Corneal distortion and higher-order aberrations due to keratoconus may contribute to halos and glare, usually more noticeable at night.
-
Vision that is not crisp
Irregular astigmatism related to keratoconus makes vision correction difficult with glasses. Further investigate poor quality of vision to rule out ocular disease.
-
iDetective’s Notes
Even with 20/20 vision, the presence of glare or shadows may indicate ocular pathology from the front or back of the eye. Suspect keratoconus in young individuals with worsening visual complaints in the absence of cataracts and retinal disease.
-Dr Chiu, iDetective
Retinoscopy and
Ophthalmoscopy Signals
Scissor reflex with retinoscopy
In one study, retinoscopy was found to have 98% sensitivity and 78% specificity when compared with Pentacam’s Belin/Ambrósio Display Final D index of ≥2.69.1
Charleaux “oil droplet” sign with direct ophthalmoscopy
If a patient has keratoconus, a total internal reflection of light due to the conical cornea may produce the oil droplet reflex.
Reference
- Al-Mahrouqi H, Oraba SB, Al-Habsi S, et al. Retinoscopy as a screening tool for keratoconus. Cornea. 2019;(4):442-445.
When suspecting keratoconus, we can’t forget that retinoscopy or direct ophthalmoscopy can be incredibly helpful to aid in keratoconus detection, especially if you don’t have a topographer.
Retinoscopy and
Ophthalmoscopy Signals



From the Case Files of
iDetective Bobby “Eye Spy KC” Saenz
OD, MS, FAAO
iDetective’s Notes:
When suspecting keratoconus, we can’t forget that retinoscopy or direct ophthalmoscopy can be incredibly helpful to aid in keratoconus detection, especially if you don’t have a topographer.
From the case files of iDetective
Bobby “Eye Spy KC” Saenz
OD, MS, FAAO
Retinoscopy and
Ophthalmoscopy Signals
-
Scissor reflex with retinoscopy
In one study, retinoscopy was found to have 98% sensitivity and 78% specificity when compared with Pentacam’s Belin/Ambrósio Display Final D index of ≥2.69.1
-
Charleaux “oil droplet” sign with direct ophthalmoscopy
If a patient has keratoconus, a total internal reflection of light due to the conical cornea may produce the oil droplet reflex.
-
iDetective’s Notes
When suspecting keratoconus, we can’t forget that retinoscopy or direct ophthalmoscopy can be incredibly helpful to aid in keratoconus detection, especially if you don’t have a topographer.
-Dr Saenz, iDetective
-
Reference
- Al-Mahrouqi H, Oraba SB, Al-Habsi S, et al. Retinoscopy as a screening tool for keratoconus. Cornea. 2019;(4):442-445.

Topographic
Irregularities
Asymmetry on topography
Keratoconus is a disease of corneal asymmetry. An example of asymmetry that may indicate keratoconus is when the I-S ratio is >1.5 D. The I-S ratio is the inferior-superior dioptric asymmetry value—the numerical differences between the average Ks in the inferior hemisphere and the superior hemisphere. Asymmetry between eyes (Kmax or average K ≥1.00 D) is an important clue.
Skewed radial axis (SRAX) or irregular astigmatism on topography
Keratoconus is a disease causing the development of nonorthogonal (irregular) astigmatism over time. Any SRAX >10 degrees, and/or subsequent increases in SRAX over time, may indicate corneal ectasia.
Increase in steepest K or Kmax
Keratometry should not significantly change over time in healthy patients. Increases in curvature >1.00 D may indicate biomechanical weakness (ectasia) and should be further investigated using tomography or topography, and then monitored for further progression.
Corneal asymmetry (I-S ratio >1.5 D), irregularity (SRAX >10 degrees) or increase in K readings (≥1.00 D) over time require further evaluation with corneal tomography to rule out keratoconus. Additionally, Kmax or steepest K >47.00 D and unexplained BCVA worse than 20/20 require further investigation with corneal tomography. Keratoconus is a disease of asymmetry, so always compare findings with the other eye.
Topographic
Irregularities



From the Case Files of
iDetective Bill “Bond” Tullo
OD, FAAO
iDetective’s Notes:
Corneal asymmetry (I-S ratio >1.5 D), irregularity (SRAX >10 degrees) or increase in K readings (≥1.00 D) over time require further evaluation with corneal tomography to rule out keratoconus. Additionally, Kmax or steepest K >47.00 D and unexplained BCVA worse than 20/20 require further investigation with corneal tomography. Keratoconus is a disease of asymmetry, so always compare findings with the other eye.
From the case files of iDetective
Bill “Bond” Tullo
OD, FAAO
Topographic
Irregularities
-
Asymmetry on topography
Keratoconus is a disease of corneal asymmetry. An example of asymmetry that may indicate keratoconus is when the I-S ratio is >1.5 D. The I-S ratio is the inferior-superior dioptric asymmetry value—the numerical differences between the average Ks in the inferior hemisphere and the superior hemisphere. Asymmetry between eyes (Kmax or average K ≥1.00 D) is an important clue.
-
Skewed radial axis (SRAX) or irregular astigmatism on topography
Keratoconus is a disease causing the development of nonorthogonal (irregular) astigmatism over time. Any SRAX >10 degrees, and/or subsequent increases in SRAX over time, may indicate corneal ectasia.
-
Increase in steepest K or Kmax
Keratometry should not significantly change over time in healthy patients. Increases in curvature >1.00 D may indicate biomechanical weakness (ectasia) and should be further investigated using tomography or topography, and then monitored for further progression.
-
iDetective’s Notes
Corneal asymmetry (I-S ratio >1.5 D), irregularity (SRAX >10 degrees) or increase in K readings (≥1.00 D) over time require further evaluation with corneal tomography to rule out keratoconus. Additionally, Kmax or steepest K >47.00 D and unexplained BCVA worse than 20/20 require further investigation with corneal tomography. Keratoconus is a disease of asymmetry, so always compare findings with the other eye.
-Dr Tullo, iDetective
Down Syndrome
Higher predisposition to keratoconus
Studies have shown that the risk of keratoconus is at least 10 times greater in the Down syndrome population.1
Patients who rub their eyes aggressively
You may observe that patients with Down syndrome who also have keratoconus frequently rub their eyes.
Objective tests
An autorefractor/ keratometer and retinoscopy are quick and effective tools for uncovering keratoconus warning signs in patients who may be less likely to report changes in vision.
Reference
- Alio JL, Vega-Estrada A, Sanz P, et al. Corneal morphologic characteristics in patients with Down Syndrome. JAMA Ophthalmol. 2018;136(9)971-978.
Keratoconus must be ruled out in patients with Down syndrome. Due to the increased incidence coupled with an even worse keratoplasty prognosis in a patient with Down syndrome, this group of patients should have a yearly topography or tomography.
Down Syndrome


From the Case Files of
iDetective Mitch “Private Eye” Ibach
OD, FAAO
iDetective’s Notes:
Keratoconus must be ruled out in patients with Down syndrome. Due to the increased incidence coupled with an even worse keratoplasty prognosis in a patient with Down syndrome, this group of patients should have a yearly topography or tomography.
From the case files of iDetective
Mitch “Private Eye” Ibach
OD, FAAO
Down Syndrome
-
Higher predisposition to keratoconus
Studies have shown that the risk of keratoconus is at least 10 times greater in the Down syndrome population.1
-
Patients who rub their eyes aggressively
You may observe that patients with Down syndrome who also have keratoconus frequently rub their eyes.
-
Objective tests
An autorefractor/ keratometer and retinoscopy are quick and effective tools for uncovering keratoconus warning signs in patients who may be less likely to report changes in vision.
-
iDetective’s Notes
Keratoconus must be ruled out in patients with Down syndrome. Due to the increased incidence coupled with an even worse keratoplasty prognosis in a patient with Down syndrome, this group of patients should have a yearly topography or tomography.
-Dr Ibach, iDetective
-
Reference
- Alio JL, Vega-Estrada A, Sanz P, et al. Corneal morphologic characteristics in patients with Down Syndrome. JAMA Ophthalmol.2018;136(9)971-978.
Connective Tissue Disorders
Collagen disorders
Because the cornea is composed of collagen, keratoconus may be a manifestation of an underling systemic condition.1
Ehlers-Danlos syndromes (EDS)
It has been recently reported that patients with EDS may have a genetic predisposition to keratoconus; the association between the two conditions has been previously suggested.2
Marfan syndrome
Marfan syndrome is responsible for reduced collagen strength affecting the eyes, bones and joints, skin, lungs, and heart. Patients with Marfan syndrome may have corneas that are soft and weak.3
References
- Beene LC, Traboulsi EI, Seven I, et al. Corneal deformation response and ocular geometry: a noninvasive diagnostic strategy in Marfan syndrome. Am J Ophthalmol. 2016;161:56-64.
- Fransen E, Valgaeren H, Janssens K, et al. Resequencing of candidate genes for keratoconus reveals a role for Ehlers–Danlos Syndrome genes. Eur J Hum Genet. 2021;29(12):1745-1755.
- Kara N, Bozkurt E, Baz O, et al. Corneal biomechanical properties and intraocular pressure measurement in Marfan patients. J Cataract Refract Surg. 2012;38(2):309-314.
Attention to patient history and reports on connective tissue disorders should alert you to be attentive for signs of ocular manifestations including keratoconus.
Connective Tissue Disorders



From the Case Files of
iDetective Tracy “Tracker” Swartz
OD, MS, FAAO
iDetective’s Notes:
Attention to patient history and reports on connective tissue disorders should alert you to be attentive for signs of ocular manifestations including keratoconus.
From the case files of iDetective
Tracy “Tracker” Swartz
OD, MS, FAAO

Connective Tissue Disorders
-
Collagen disorders
Because the cornea is composed of collagen, keratoconus may be a manifestation of an underling systemic condition.1
-
Ehlers-Danlos syndromes (EDS)
It has been recently reported that patients with EDS may have a genetic predisposition to keratoconus; the association between the two conditions has been previously suggested.2
-
Marfan syndrome
Marfan syndrome is responsible for reduced collagen strength affecting the eyes, bones and joints, skin, lungs, and heart. Patients with Marfan syndrome may have corneas that are soft and weak.3
-
iDetective’s Notes
Attention to patient history and reports on connective tissue disorders should alert you to be attentive for signs of ocular manifestations including keratoconus.
-Dr Schroeder Swartz, iDetective
-
References
- Beene LC, Traboulsi EI, Seven I, et al. Corneal deformation response and ocular geometry: a noninvasive diagnostic strategy in Marfan syndrome. Am J Ophthalmol. 2016;161:56-64.
- Fransen E, Valgaeren H, Janssens K, et al. Resequencing of candidate genes for keratoconus reveals a role for Ehlers–Danlos Syndrome genes. Eur J Hum Genet. 2021;29(12):1745-1755.
- Kara N, Bozkurt E, Baz O, et al. Corneal biomechanical properties and intraocular pressure measurement in Marfan patients. J Cataract Refract Surg. 2012;38(2):309-314.

Contact Lens
Considerations
Instability with toric soft lenses
Corneal ectasia causes irregular astigmatism, which makes correction in toric soft contact lenses difficult. If fit and vision are unstable, consider keratoconus screening.
Improved clarity with rigid contact lenses
If rigid gas-permeable, hybrid, or scleral lenses significantly improve vision compared with glasses or soft contact lenses, it might be due to an irregular cornea or keratoconus.
Corneal molding effect
Rigid lenses that touch the cornea may temporarily flatten the cornea. Topography taken immediately after lens removal may not be accurate and might mask keratoconus progression.
While soft lenses may work well for early keratoconus, specialty lenses are typically required to achieve best corrected vision in more advanced cases. With early detection and treatment to minimize progression, quality of vision might be preserved with even glasses or soft contact lenses.
Contact Lens
Considerations




From the Case Files of
iDetective Gloria “Gadget” Chiu
OD, FAAO, FSLS
iDetective’s Notes:
While soft lenses may work well for early keratoconus, specialty lenses are typically required to achieve best corrected vision in more advanced cases. With early detection and treatment to minimize progression, quality of vision might be preserved with even glasses or soft contact lenses.
From the case files of iDetective
Gloria “Gadget” Chiu
OD, FAAO, FSLS

Contact Lens
Considerations
-
Instability with toric soft lenses
Corneal ectasia causes irregular astigmatism, which makes correction in toric soft contact lenses difficult. If fit and vision are unstable, consider keratoconus screening.
-
Improved clarity with rigid contact lenses
If rigid gas-permeable, hybrid, or scleral lenses significantly improve vision compared with glasses or soft contact lenses, it might be due to an irregular cornea or keratoconus.
-
Corneal molding effect
Rigid lenses that touch the cornea may temporarily flatten the cornea. Topography taken immediately after lens removal may not be accurate and might mask keratoconus progression.
-
iDetective’s Notes
While soft lenses may work well for early keratoconus, specialty lenses are typically required to achieve best corrected vision in more advanced cases. With early detection and treatment to minimize progression, quality of vision might be preserved with even glasses or soft contact lenses.
-Dr Chiu, iDetective
Abnormal Slit
Lamp Examination
Fleischer ring
Fleischer ring is an iron ring within the epithelium at the base of the cone. It is brown in color and best visualized using the cobalt blue filter.
Vogt striae
If you suspect keratoconus, look for vertical lines within
the posterior stroma or Descemet membrane.
Stromal thinning
Stromal thinning is often present in the cone. It may initially be subtle, but it can become more pronounced over time.
In the CLEK study of 1209 KC patients, 86% of the subjects presented with a Fleischer ring; 65% with Vogt striae; and 53% with scarring. If any of these are seen, suspect keratoconus. Munson sign (protrusion of the lower eyelid upon downgaze) generally does not manifest until severe keratoconus, if at all.
Abnormal Slit
Lamp Examination




From the Case Files of
iDetective Susan “Super Sleuth” Gromacki
OD, MS, FAAO, FSLS
iDetective’s Notes:
In the CLEK study of 1209 KC patients, 86% of the subjects presented with a Fleischer ring; 65% with Vogt striae; and 53% with scarring. If any of these are seen, suspect keratoconus. Munson sign (protrusion of the lower eyelid upon downgaze) generally does not manifest until severe keratoconus, if at all.
From the case files of iDetective
Susan “Super Sleuth” Gromacki
OD, MS, FAAO, FSLS

Abnormal Slit
Lamp Examination
-
Fleischer ring
Fleischer ring is an iron ring within the epithelium at the base of the cone. It is brown in color and best visualized using the cobalt blue filter.
-
Vogt striae
If you suspect keratoconus, look for vertical lines within the posterior stroma or Descemet membrane.
-
Stromal thinning
Stromal thinning is often present in the cone. It may initially be subtle, but it can become more pronounced over time.
-
iDetective’s Notes
In the CLEK study of 1209 KC patients, 86% of the subjects presented with a Fleischer ring; 65% with Vogt striae; and 53% with scarring. If any of these are seen, suspect keratoconus. Munson sign (protrusion of the lower eyelid upon downgaze) generally does not manifest until severe keratoconus, if at all.
-Dr Gromacki, iDetective
Discover iLink: FDA-approved cross-linking procedure for progressive keratoconus
Chat with the Detective
Uncover expert insights on all things keratoconus and find answers to your questions about the condition.
Use these tools to help crack the case of keratoconus
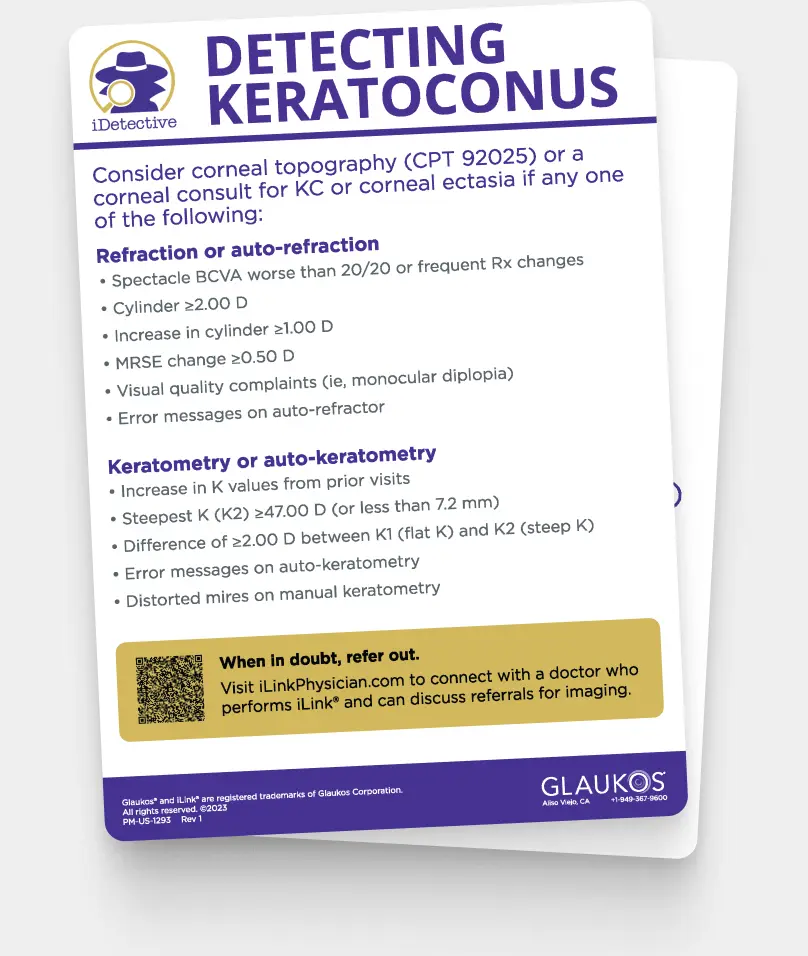
Auto-refractor Card
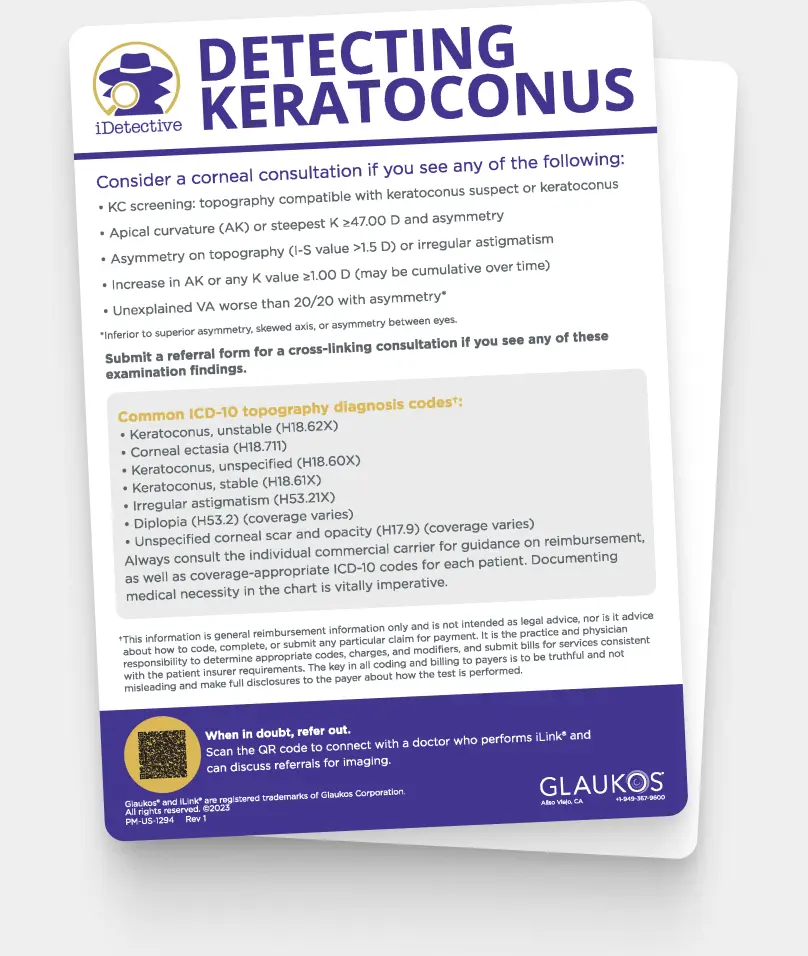
Topographer Card
All Resources
Master in KC detection and referral
Find out how you can
continue to care for patients
after cross-linking
Contact us today with any questions you have about the iDetective program
Request More Info
"*" indicates required fields